Today we’re focusing on a critical update from the 2026 Home Health Proposed Rule: the introduction of a new measure to the Value-Based Purchasing (VBP) program, effective in 2026 if the rule is finalized as written. This measure, the “Medicare Spending Per Beneficiary Post-Acute Care Measure” (MSPB-PAC), is designed to encourage agencies to strengthen care coordination and accountability.
To help us understand this significant change, we’ll break down the key components of the MSPB-PAC calculation.
What is the MSPB-PAC Measure?
The MSPB-PAC measure is a claims-based tool that assesses cost and resource use by tracking the expenses Medicare incurs for services provided to each beneficiary in post-acute care. This measure has been a part of the Home Health Quality Reporting Program (HHQRP) since 2017 and is also used across other post-acute care settings, including Inpatient Rehabilitation Facilities (IRF), Long-Term Acute Care Hospitals (LTACH), and Skilled Nursing Facilities (SNF). For home health, it evaluates an agency’s performance against the national median for the same performance period.
A key distinction for home health is that the MSPB-PAC is calculated based on an “episode of care,” while in other post-acute settings, it’s measured by a “stay.”
How is the Calculation Determined?
The calculation of this measure involves a few steps and relies on two years of data, with each future performance year based on a single, non-overlapping year.
The formula is:
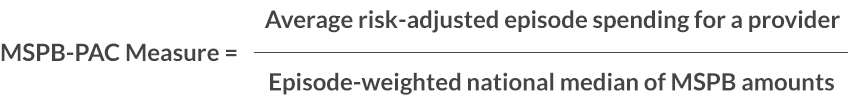
- The Numerator represents the average spending for all of an agency’s episodes. It is determined by calculating the average ratio of standardized episode spending to expected episode spending, then multiplying that by the national average episode spending across all home health providers.
- The Denominator is the episode-weighted national median of MSPB amounts across all home health providers, serving as the benchmark for comparison.
Understanding “Episodes”
For the purpose of this measure, an “episode” refers to all Medicare Part A and Part B services provided within a defined episode window. This window begins on the first day of a home health claim, which marks the start of the treatment period.
Home health episodes are grouped into three distinct types for calculation:
- Standard Episode: Begins with a home health claim that does not involve a LUPA (Low Utilization Payment Adjustment) or PEP (Partial Episode Payment) adjustment.
- LUPA Episode: Occurs when a home health claim meets the criteria for a LUPA episode.
- PEP Episode: A PEP adjustment is applied when a home health claim qualifies for a prorated payment due to a shortened care period. This happens when a patient is discharged and then readmitted, either to the same or a different agency, without a 60-day gap between discharge and readmission. If a claim qualifies for both a PEP and LUPA, it is categorized as a PEP episode.
Importantly, MSPB-PAC episodes are evaluated only against episodes of the same type. This means LUPA episodes are compared with other LUPA episodes, and PEP episodes are compared with other PEP episodes, rather than lumping all episode types together.
The “Attributed Provider’s Episode” encompasses both the home health treatment period and all related services. For instance, if a patient has a hospital stay while under an agency’s care, those costs are counted toward the agency’s overall spending for the episode.
This new measure will push agencies to focus on more efficient care coordination, ensuring patients receive the right services at the right time, thereby reducing unnecessary costs. This is not just about cutting expenses; it’s about improving patient outcomes and preventing avoidable hospitalizations.
CodingDepartmenet.com is ready to support you in navigating these and other upcoming changes to the Home Health Value-Based Purchasing program. For any assistance, please don’t hesitate to reach out to us.